Juvenile Arthritis
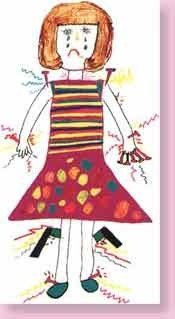
Juvenile arthritis is a general term describing various types of arthritis that may occur between birth and 16 years of age.
Arthritis can cause pain, stiffness, swelling and often inflammation in one or more joints. Around one in every 1,000 children have some form of juvenile arthritis.
The cause of juvenile arthritis is not known. Genes are thought to cause or contribute to some types. Lifestyle factors or triggers have also been found to explain why arthritis occurs in some children.
Prevention is not possible since the cause is not known. But appropriate medication, physiotherapy and a home program of stretches and strengthening exercises can make symptoms manageable and improve quality of life substantially.
Common types of juvenile arthritis include:
- Oligoarthritis
- Polyarticular arthritis (rheumatoid factor negative)
- Polyarticular arthritis (rheumatoid factor positive)
- Enthesitis arthritis
- Psoriatic arthritis
- Ankylosing Spondylitis
Symptoms of juvenile arthritis can include:
- Joint pain
- Joint swelling
- Joint stiffness
- Fever and general feeling of being unwell
- Skin rashes
- Anaemia
- Vision problems
- Eye Inflammation
- Fatigue
Diagnosis Methods
- Medical history
- Physical examination
- Blood tests
- X-rays
- Eye examination
Treatment and Management Options
In most cases early diagnosis and treatment means a good outlook for the child with juvenile arthritis. Doctors, nurses, physiotherapists, occupational therapists, dietitians, podiatrists, psychologists and social workers may all be a part of the team that treats the child.
Treatments may include:
- Physiotherapy to strengthen muscles, keep the joints flexible and encourage normal limb development
- Hydrotherapy to relieve pain and maintain joint and muscle flexibility
- Medications such as NSAIDs (non-steroid anti-inflammatory drugs) and DMARDs (disease modifying anti rheumatoid drugs) to reduce inflammation in the affected joints and avoid long-term damage to those joints
- New medications called biologics and DMA's are sometimes used for more severe cases
- Analgesics are used to treat pain
- Steroids
Where to get help?
- Your GP
- A Paediatric Rheumatologist
- Physiotherapist
Physiotherapy management includes
- Providing the child and their family with education on effective stretching and movement techniquesto keep mobile
- Core stability and pelvic stability exercises to support the painful joints
- Postural exercises to prevent disfigurement or change in back shape
- Flexible bracing in short term to encourage posture maintenance
- Hydrotherapy to relieve pain and stretch out stiff joints and tight muscles
- Advice on pacing of activity and ensuring adequate rest and relaxation
- Helping the child work determine more suitable gentle forms of exercise during flare-ups that will still enable child to maintain good social contact with friends and peers